Healthcare providers and people with Medicare will be able to use secure look-up tools that will allow quick access to the new Medicare numbers when needed. There will also be a 21-month transition period where doctors, healthcare providers, and suppliers will be able to use either their current SSN-based Medicare Number or their new, unique Medicare number, to ease the transition.
Covered California: Marketing and Outreach to Stabilize the Individual Market Report
“A comprehensive marketing and outreach campaign has been a critical ingredient of Covered California’s success, and more importantly is a vital component of any effort to promote stability in individual markets across the nation,” said Lee. “Getting the word out is a proven way to promote enrollment and bring more healthy people into the risk pool, which lowers premiums and saves money for everyone.”
Blue Shield To Close Grandfathered And Popular Plans In 2018
The membership of our grandfathered plans continues to get smaller every year. When a plan’s membership drops below 500 members, we need to review our portfolio and consider changes that benefit all Blue Shield members. Therefore, we are withdrawing the following Blue Shield of California grandfathered plans from the Individual and Family Plans market.
Medi-Cal To Treat Same-Sex Spouses The Same As Opposite-Sex Spouses
The Department of Health Care Services notified all county welfare directors in a letter dated July 31, 2017, that for eligibility determinations, same-sex married couples will be treated the same as opposite-sex married spouses. One of the significant changes is that county eligibility workers will no longer have to request verification of the same-sex marriage. They same-sex couple, regardless of which state they were married in, will just have to attest under penalty of perjury that they are legally married.
WHA Expands To Bay Area, But Leaves Covered California
Western Health Advantage (WHA) has announced that the Department of Managed Health Care has approved their expansion for small group plans into the Bay Area. They also noted that they will not seek re-certification of their Covered California small group plans because of this expansion. WHA’s exit from the Covered California for Small Business plans does not affect their individual and family plan offerings through Covered California.
Confusion Over Medicare and Obamacare Enrollment, CMS Waives Late Enrollment Part B Penalty
CMS is offering equitable relief to certain individuals enrolled in both Medicare Part A and coverage through the Marketplace for individuals and families to enroll in Medicare Part B without penalty. Further, CMS is offering equitable relief to certain individuals who dropped or lost their coverage through the Marketplace and are paying a late enrollment penalty from their subsequent late enrollment into Medicare Part B. These eligible individuals can have their penalty reduced. Individuals can apply for the Medicare Part B enrollment opportunity and reduction in late enrollment penalties during a limited time – it is available now and ends September 30, 2017.
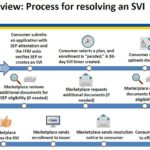
Healthcare.gov Special Enrollment Verification Phase II: Marriage, Adoption, Medicaid
After a consumer has submitted an application under the Special Enrollment Period with a qualifying event, and then selects a health plan, the consumer will have 30 days to verify the qualifying event. The consumer can upload or mail the documentation verifying the qualifying event. The Marketplace will review the documentation and request additional information if necessary.
Blue Cross Mailing Letters To Californians With Terminated Plan For 2018
In order to give members impacted by this change plenty of time to plan for their coverage needs in 2018, we are notifying affected members over the next few days that their current plan will be discontinued on December 31, 2017. This includes all on and off exchange members outside of rating regions 1, 7 and 10, and HMO members in rating region 7. It’s important to note that until 2018, their coverage stays the same. All they need to do is keep paying their premiums.
California works to combat Trump’s undermining of the ACA
Thanks to the actions of President Trump, in April I took the unprecedented step authorizing health insurers to file two sets of rates for 2018,” said Insurance Commissioner Dave Jones. “We in California are doing everything we can to keep carriers and plans in the individual market, but President Trump continues to undermine the ACA and as these rate filings demonstrate, California is not immune to his efforts to wreck the Affordable Care Act. If President Trump continues down this path, premiums will increase substantially in 2018. The average premium increase doubles if Trump continues to refuse to fund the cost-sharing assistance in the ACA.
Anthem adjusts Individual health plan offerings in California for 2018
Next year, we will offer plans in three regions of Northern California only, which will include Redding, Santa Clara County, and Stockton/Modesto. The coverage options will include EPO plans available both on-exchange and off-exchange, and at all metal levels. Staying in these three key areas will help ensure Californians in those regions have access to health plans.
- « Previous Page
- 1
- 2
- 3
- 4
- 5
- 6
- …
- 38
- Next Page »