Blue Shield released information and documents relating to their California individual and family plans (IFP) for 2016. They have dropped their 2015 Exclusive Provider Organization (EPO) plans that offered no out-of-network coverage. All Blue Shield of California IFPs will be PPO with their Exclusive PPO Network of providers. Blue Shield will also be expanding coverage areas to offer plans in the counties of Alpine, Monterey, Sutter and Yuba counties in 2016.
Anthem Blue Cross California releases 2016 individual and family plan material
The exclusive provider organization (EPO) is now a tiered preferred provider organization (PPO) plan. Members on 2015 EPO plans will be transitioned to Tiered PPO plans effective 1/1/16 (unless they choose a different plan).
IRS facts on letters regarding 1095-A and tax returns
The IRS sent letters to taxpayers this summer who were issued a Form 1095-A, Health Insurance Marketplace Statement, showing that advance payments of the premium tax credit were paid on the taxpayer’s behalf in 2014. At the time, the IRS had no record that the taxpayer filed a 2014 tax return.
Health Net special coverage for victims of California wildfires
Health Net is helping ensure that its members who have lost their homes or been evacuated due to any of the current wildfires in California, Oregon and Washington have access to essential prescription medications, critical Health Net information and other services to help them cope with grief, loss, stress or trauma.
Kaiser to release new billing system in California
Kaiser Permanente for Individuals and Families (KPIF) has a new billing system for plan members to access and pay their bills. Clients’ premium bills, payment stubs, and online payment portal will have a new look. We have new contact information.
What employee information must employers report to the IRS?
What Information Must a Health Coverage Provider Report to the IRS?
Health plans may ask for your Social Security number
Your health insurance company may request that you provide them with the social security numbers for you, your spouse and your children covered by your policy. This is because the Affordable Care Act requires every provider of minimum essential coverage to report that coverage by filing an information return with the IRS and furnishing a statement to covered individuals. The information is used by the IRS to administer – and individuals to show compliance with – the health care law.
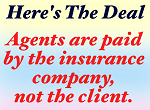
Agents paid $9.2 M monthly on IFP Covered California enrollments
Covered California enrollments assisted by Certified Insurance Agents are producing a minimum of $9.2 million per month in commissions as estimated from enrollment statistics released by the states ACA exchange. While this number may sound impressive, a good chunk of the enrollments were for individuals and families who already had health insurance. With many health […]