CMS is offering equitable relief to certain individuals enrolled in both Medicare Part A and coverage through the Marketplace for individuals and families to enroll in Medicare Part B without penalty. Further, CMS is offering equitable relief to certain individuals who dropped or lost their coverage through the Marketplace and are paying a late enrollment penalty from their subsequent late enrollment into Medicare Part B. These eligible individuals can have their penalty reduced. Individuals can apply for the Medicare Part B enrollment opportunity and reduction in late enrollment penalties during a limited time – it is available now and ends September 30, 2017.
Healthcare.gov Special Enrollment Verification Phase II: Marriage, Adoption, Medicaid
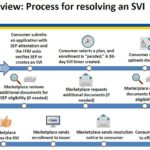
After a consumer has submitted an application under the Special Enrollment Period with a qualifying event, and then selects a health plan, the consumer will have 30 days to verify the qualifying event. The consumer can upload or mail the documentation verifying the qualifying event. The Marketplace will review the documentation and request additional information if necessary.
Trump Watches As Health Insurance Ship Sinks
“This is yet another failing report card for the Exchanges. The American people have fewer insurance choices and in some counties no choice at all. CMS is working with state departments of insurance and issuers to find ways to provide relief and help restore access to healthcare plans, but our actions are by no means a long-term solution to the problems we’re seeing with the Insurance Exchanges,” said CMS Administrator Seema Verma.
Insurance Commissioner Jones Bashes Repeal of ACA House Vote
“Today’s Republican House vote will rob 24 million Americans of health care coverage, which is tantamount to a death sentence for some patients who depend on coverage to manage serious and chronic medical conditions. The President and House Republicans have nothing to be proud of today as they work to take health care coverage away from millions of Americans who will be harmed by their actions.
ACA Proposed Rule Changes for 2018
This rule proposes changes that would help stabilize the individual and small group markets. This proposed rule would amend standards relating to special enrollment periods, guaranteed availability, and the timing of the annual open enrollment period in the individual market for the 2018 plan year; standards related to network adequacy and essential community providers for qualified health plans; and the rules around actuarial value requirements.
Department of Insurance Receives Health Plan Compliance Grant
The Centers for Medicare and Medicaid Services at the U.S. Department of Health & Human Services announced today it awarded a $1.84 million grant to the California Department of Insurance to enhance enforcement of key market reforms under the Affordable Care Act.
Moving won’t guarantee health insurance enrollment
New rules limit the circumstances in which someone may qualify for the permanent move SEP to ensure consistency with the original purpose of that SEP. An Interim Final Rule with Comment (IFC) published in the Federal Register provides that individuals requesting a “permanent move” SEP must have minimum essential coverage for one or more days in the 60 days preceding the permanent move, unless they were living outside of the United States or in a United State territory prior to the permanent move. This ensures that individuals are not moving for the sole purpose of obtaining health coverage outside of the open enrollment period.
Incarceration status and health insurance subsidies
The Centers for Medicare and Medicaid Services has released a Frequently Ask Questions documents discussing health insurance subsidies when a person is incarcerated in jail or prison. This includes such situations of a person being arrested but not yet convicted of a crime and those on probation and parole.
Home Health Care Company Ratings and Comparisons
The Centers for Medicare & Medicaid Services (CMS) introduced the first patient experience of care star ratings on Home Health Compare. Known as Home Health Care Consumer Assessment of Healthcare Providers and Systems (HHCAHPS) Survey star ratings, these measures evaluate patients’ experiences with home health agencies.
Some qualifying events eliminated for Special Enrollment Periods
Elimination of several unnecessary special enrollment periods, clarifies the definitions of other special enrollment periods, and provides stronger enforcement so that special enrollment periods serve the purpose for which they are intended and do not provide unintended loopholes.