
Sutter Health Plus
2017 Evidence of Coverage and Disclosure Form (EOC) and Benefit Plan Design Changes for Sutter Health Plus Individual Family Plans, Small Group and Large Group Plans.
- Plan design changes to some Individual Family Plans and Small and Large Group plans to comply with parity requirements in the Mental Health Parity and Addiction Equity Act (MHPAEA)
- Changes to the 2017 EOC Section III, for Individual Family Plans, Small Group and Large Group plans that recently received approval from the Department of Managed Health Care (DMHC).
-
Mental Health/Substance Use Disorder Benefits
These benefit changes will reduce member cost share for Mental Health, Behavioral Health and Substance Use Disorder (MH/SUD) and emergency medical transportation benefits. Previously filed claims will be retroactively adjusted back to dates of service on or after January 1, 2016. Members who paid the incorrect cost sharing amount will receive a separate letter and refund, as appropriate.
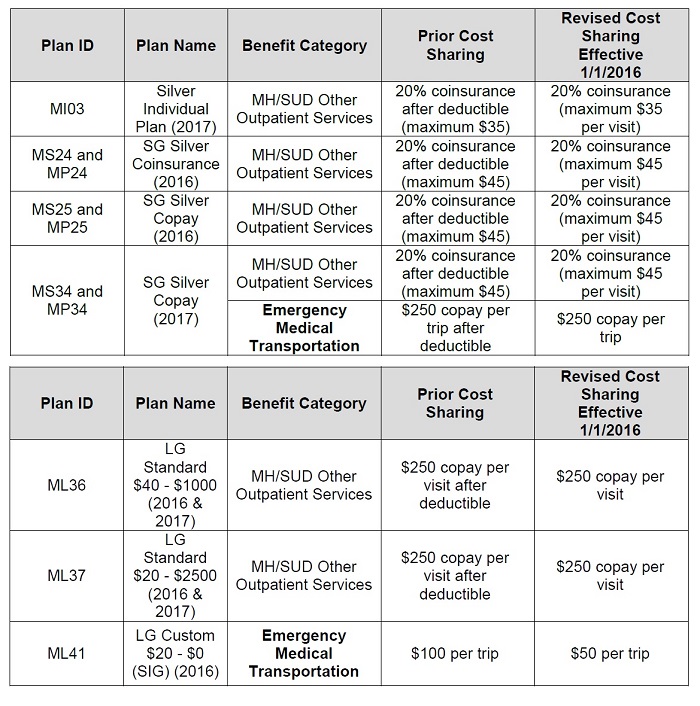
Sutter Health changes to 2017 Evidence of Coverage for Mental Health and Substance Abuse benefits for individual and family, small group, and large group plans.
-
2017 Evidence of Coverage and Disclosure Form (EOC), Section III, for Individual Family Plans, Small Group and Large Group Plans
Individual Family Plans
Additional Changes and Clarification of EOC Language
- Sutter Health Plus revised the Prior Authorization section in the Seeing a Doctor and Other Providers chapter on page 20 to add services for reproductive or sexual health care to the list of services that do not require a referral from a member’s primary care physician
- Sutter Health Plus added a Timely Access to Care section on page 28 that provides information regarding appointment wait times for urgent care, non-urgent primary care, non-urgent specialty care and telephone screenings
- Sutter Health Plus revised the language in the Outpatient Prescription Drugs, Supplies, Equipment and Services section in the Your Benefits chapter on page 59 to state that FDA-approved, self-administered hormonal contraceptives dispensed at one time for a member by a provider, pharmacist, or location licensed or authorized to dispense drugs or supplies may be covered at up to a 12-month supply
- Sutter Health Plus revised the Preventive Care benefit on page 33 for screening flexible sigmoidoscopies and colonoscopies to be more broadly described as colorectal cancer screening
- Sutter Health Plus revised the Health Education section on pages 42 and 43 to clarify the coverage for health education services
- Sutter Health Plus revised the Service Area Eligibility Requirements section on page 11 and removed the reference to place of work as an eligibility requirement
- Sutter Health Plus revised the pediatric and dental benefit language throughout the EOC to reflect that pediatric vision and dental care benefits are for individuals until at least the end of the month in which the enrollee turns 19 years of age, not for individuals under 19 years of age
Small Group and Large Group Plans
Changes and Clarification of EOC Language
- Sutter Health Plus added a Timely Access to Care section to the Seeing a Doctor and Other Providers chapter that provides information regarding appointment wait times for urgent care, non-urgent primary care, non-urgent specialty care and telephone screenings
- Sutter Health Plus revised the Preventive Care benefit for screening flexible sigmoidoscopies and colonoscopies in the Your Benefits chapter to be more broadly described as colorectal cancer screening
- Sutter Health Plus revised the Health Education Services section in the Your Benefits chapter to clarify the coverage for health education services
- In the Small Group EOCs, Sutter Health Plus revised the pediatric and dental benefit language throughout the EOC to reflect that pediatric vision and dental care benefits are for individuals until at least the end of the month in which the enrollee turns 19 years of age, not for individuals under 19 years of age