
Health Net
Introducing Advanced Choice Pharmacy Network
New, tailored pharmacy network designed for cost control
At Health Net, we’re always on the lookout for ways to keep quality health care affordable for employers and members. Our latest focus is on pharmacy costs, currently a major premium cost driver.
Introducing Advanced Choice pharmacy network – our first tailored pharmacy network, which connects members to CVS, Walmart, Costco, Safeway, Vons, and other pharmacies. Walgreens is excluded.
Who’s impacted and when?
Advanced Choice will be paired with a select number of California Individual & Family Plans (IFP) and Small Business Group (SBG) plans. The effective dates are staggered as follows:
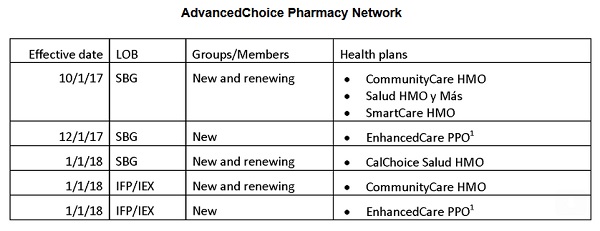
Health Net AdvancedChoice Pharmacy Network will apply to some small group and individual plans beginning as early as October 2017.
How will members and employers be notified?
Members who have used a Walgreens pharmacy at any time in the past 12 months will receive a letter about the change 60 days in advance of the end of the year if they have an individual and family plan. Group members will receive the letter 60 days in advance of their employer’s renewal date. The first letters mail late July to members of groups renewing October 1.
Employer renewal packets for Q4 renewals will also highlight the change. We’re emphasizing that members continue to have access to CVS, Walmart, Costco, Safeway, Vons, and other pharmacies, and that only Walgreens is excluded.
Clear instructions on how to find a pharmacy will also be included in both member and group communications.
Effective October 1, to find a pharmacy in the Advanced Choice network:
- Go to www.healthnet.com and choose Members, then Member Plan Information.
- Under Select Your Plan Type, choose Group Plan.
- Select Find a Pharmacy (at the bottom of the page).
- Click on Advanced Choice Pharmacy Network.
- EnhancedCare PPO is our newest medical plan innovation, which we’ll be introducing to you for 2018