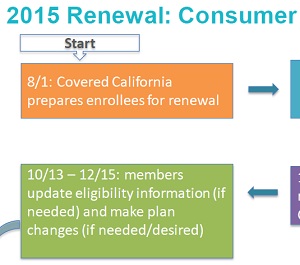
Covered California will be hosting bi-monthly webinars for agents, enrollers and navigators on the 2015 renewal and open enrollment period. The first presentation was on the
automatic enrollment for existing consumers and some of the technical issues that might occur. The webinar itself, Sales Partner Renewal Webinar October 8th 2014, was approximately 48 minutes long. While the bulk of the information is contained in the slide presentation that can down loaded at the end of the post, the narration did provide a few extra side notes to the slides.
Renewal topics included
- Most consumers will auto-renew with no action.
- Some consumers must take action to update income, household members or change plans.
- Special notices sent by Covered California to consumers in Contra Costa Health Services and Health Net plans was incorrect.
- If no action is taken by consumers in Contra Costa and Health Net PPO plans, they will lose coverage on December 31, 2014.
- Consumers who did consent to yearly verification of income must submit permission. If consumer does not grant permission to verify income they will lose the APTC as of December 31, 2014.
- Catastrophic plans for 31 year olds will renew at a Bronze level.
- Consumers who didn’t submit proper immigration or naturalization documents will lose coverage on October 31, 2014.
- CalHEERS will switch to “renewal” mode on October 13th which will most likely present problems for people trying to enroll for 2014 coverage under a SEP and potential problems with adding a new family member from a birth or adoption.