The rule includes clarifications and requirements for covered entities (including Anthem) that impact how Anthem administers benefits related to transgender services, and requires Anthem to add statements on materials provided to members about nondiscrimination, as well as information about language assistance.
Covered California to contact employers of exchange health plan members
Covered California will begin contacting employers of Covered California individuals and families notifying them that their employee is receiving Obamacare premium assistance. Only employers for whom enrolled Covered California members have provided employer contact information will be sent the notification. The letters will alert the employer that they may be subject to the employer shared responsibility payment if they have 50 or more employees.
Covered California update removes income assessment for unmarried pregnant women
Covered California will implement several changes to their online application program known at CalHEERS on August 1, 2016. One significant change is no longer assessing unmarried pregnant women’s income for determining Medi-Cal eligibility. The previous version automatically determined Medi-Cal eligibility based on a woman’s income and pregnancy status. Because Medi-Cal considers a pregnant woman a household two at a minimum, many women were tracked into Medi-Cal and not eligible for private health insurance with the subsidies.
California Hospital Quality Ratings for 2016
Today, we [Centers for Medicare and Medicaid] are updating the star ratings on the Hospital Compare website to help millions of patients and their families learn about the quality of hospitals, compare facilities in their area side-by-side, and ask important questions about care quality when visiting a hospital or other health care provider. Today’s update comes after substantive discussions with hospitals and other stakeholders to review the Overall Hospital Quality Star Rating’s methodology.
Commissioner Jones supports DOJ block of health plan mergers
I’m very pleased with the U.S. Department of Justice action today to block these mergers because they are anti-competitive and would harm consumers and businesses. As insurance commissioner of the largest insurance market in the country, I urged the DOJ to prevent both of these health insurance mergers, which if approved would have resulted in a highly concentrated, less competitive health insurance market doing irreparable harm to consumers and businesses.
Cigna files for 18% increase in California individual and family plan rates
Cigna has filed their 2017 California individual and family plan rates with the California Department of Insurance requesting overall rate increase of 18%. Cigna’s rate filing states the new 2017 health insurance premiums would affect 18,253 of their members in California.
Health Net requests 23% rate increase for 2017 California individual and family plans
The California Department of Insurance (CDI) has posted the health insurance premium rate increase requests by Health Net for their 2017 California individual and family plans. The overall increase request is 23%, with a maximum for some health plans as high as 34%. The Health Net rate increase would apply to 11,582 members currently in their PPO and EPO health plans.
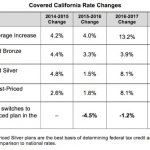
Covered California 2017 rate increases and health plan expansions
Covered California announced the rates for its health plans in the individual market for 2017. The statewide average weighted increase of 13.2 percent, while higher this year, amounts to a three-year average of 7 percent, which is less than the rate increases before the Affordable Care Act (ACA) was enacted.
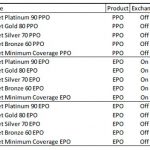
Health Net requests 15% rate increase for California small group plans
Health Net has filed new small group health insurance premium rates for 2017 with the California Department of Insurance. In the filed rates, Health Net is proposing an average expected annual increase of 15% to their PPO and EPO plans.
Blue Shield to automatically enroll members in Obamacare plans
Blue Shield of California has sent notices to 2,062 consumers of their grandfathered health plans notifying them they will be automatically enrolled in Obamacare plans for 2017. Blue Shield will no longer be offering 17 of their grandfathered individual and family plans in 2017. Blue Shield stated that the grandfathered plans are being withdrawn from the market place due to low enrollment.
- « Previous Page
- 1
- …
- 14
- 15
- 16
- 17
- 18
- …
- 38
- Next Page »