
Blue Shield of California
California Assembly Bill (AB) 72 Out-Of-Network Coverage and Member Cost-Sharing
New California law
Effective July 1, 2017, this new state law protects individuals from receiving unexpected “surprise or balance” medical bills from an out-of-network (OON) doctor when receiving inpatient and outpatient non-emergency care and services at an in-network healthcare facility such as a hospital, clinic, lab, imaging center or other healthcare facility.
Changes to out-of-network coverage and cost-sharing
When individuals go to an in-network facility for care but receive services from an out-of-network doctor or healthcare provider, they only have to pay their in-network cost-sharing amount that counts toward the annual deductible and annual out-of-pocket maximum limits according to their health plan.
An out-of-network doctor should only bill individuals after both parties have received a copy of the Explanation of Benefits (EOB) that reflects the correct in-network cost-sharing amount owed for the care received. If for any reason the out-of-network doctor or healthcare provider receives payment that is more than the cost share allowed, the out-of-network doctor must refund the overpayment within 30 days.
Below is a list of affected Blue Shield health plans.
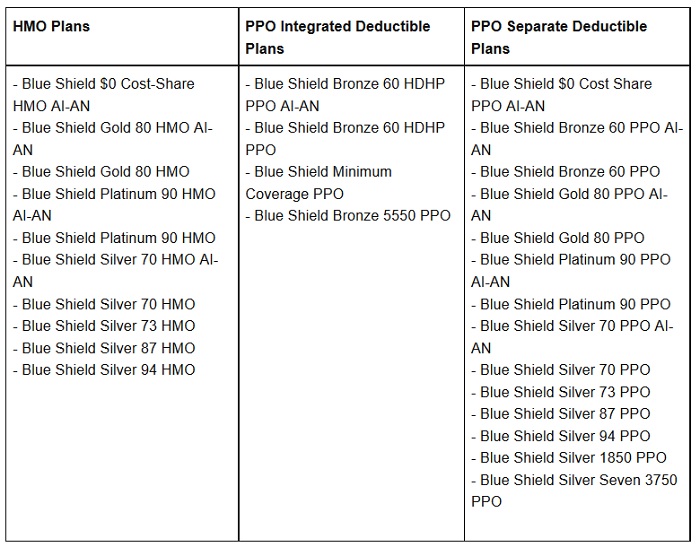
Blue Shield health plans subject to unexpected out-of-network medical billing protection.
