
Blue Shield of California
Blue Shield of California will change how out-of-network health care costs accumulate toward meeting the maximum out-of-pocket amounts for individual and family plans in 2018. They are sending letters to members discussing the details of the change which could dramatically affect some consumers. The change in how the health care costs are allocated to the in-network and out-of-network columns is in addition to sharply higher out-of-network deductibles placed on many 2018 IFP plans. To read more about the changes to out-of-network deductibles for 2018 visit https://insuremekevin.com/california-ppo-plans-come-with-high-deductibles-max-out-of-pocket-amounts/
2018 Non-Network Coverage Change Letter
Important changes to your non-network benefits
With a Blue Shield PPO plan, you have a choice of more than 46,000 doctors and 350 hospitals, plus the flexibility of seeing providers outside the network.
Starting in 2018, if you receive covered services from a provider that is not in your plan’s network, your out-of-pocket expenses will be significantly higher than they were in 2017.
In addition, any expenses you pay to see a network doctor will be counted toward your network out-of-pocket maximum, and expenses you pay to see a non-network doctor will be counted toward your non-network out-of-pocket maximum.
To make sure you get the best value, you should see doctors and use hospitals in your plan’s network.
Blue Shield web page of 2018 Changes to PPO Plans
https://www.blueshieldca.com/bsca/find-a-plan/renewal-center/whats-new-OE2018.sp
As a PPO plan member, you have the flexibility to see any doctor that you want–inside or outside your plan’s network. Starting in 2018, if you receive covered services from a provider that is not in your plan’s network, your out-of-pocket expenses will be significantly higher than they were in 2017. If the service isn’t covered, you may be responsible for all billed charges.
Blue Shield strongly encourages you to see provider’s in your plan’s network so you receive the best value and do not have to pay more out of pocket for care.
The following table shows your plan deductible and out-of-pocket maximum from 2017 to 2018 for both network and non-network providers. You can click on the table to enlarge it.
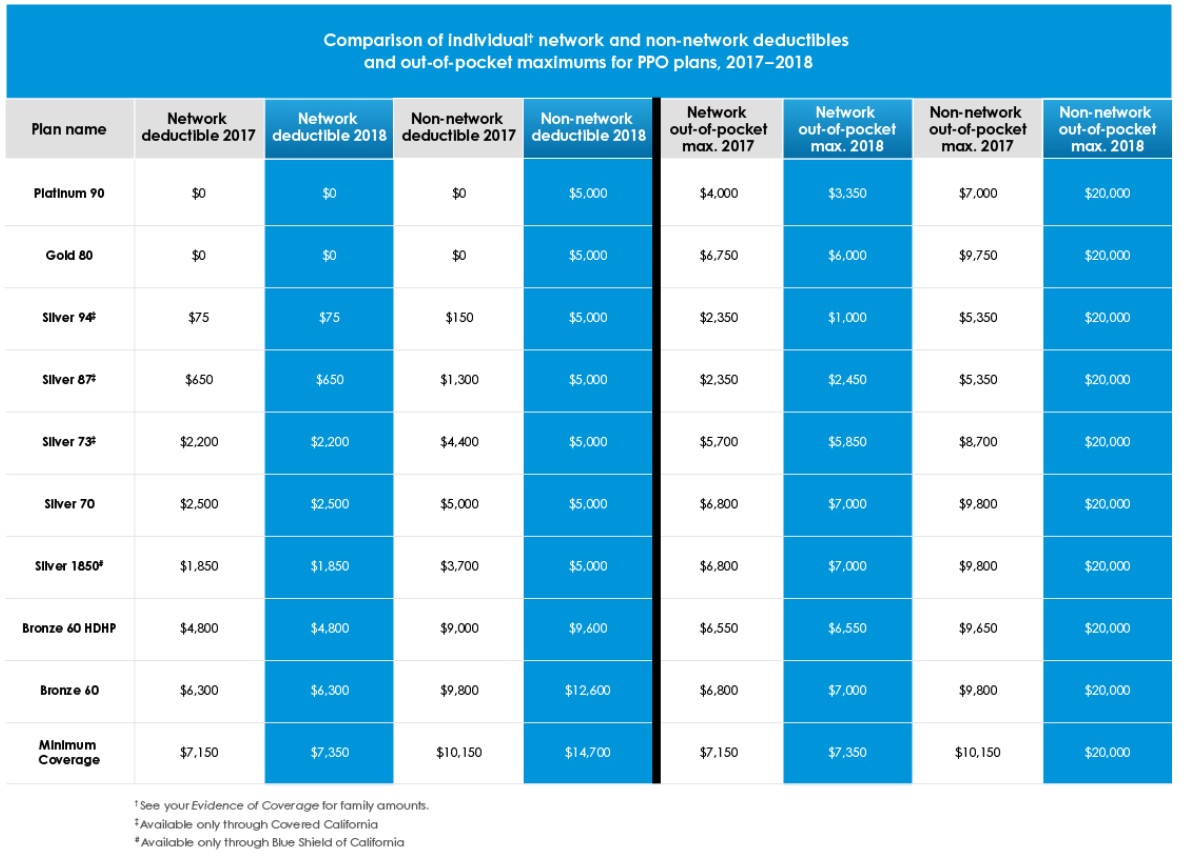
Comparison of Blue Shield PPO 2017 vs. 2018 Network and Out-of-Network deductibles and maximum out-of-pocket amount changes for individual and family plans in California.
Changes to how your out-of-pocket maximum is calculated
In addition, your out-of-pocket expenses will be counted separately for covered services received from network providers and non-network providers. Any expenses you pay to see a network doctor will be counted toward your network out-of-pocket maximum, and expenses you pay to see a non-network doctor will be counted toward your non-network out-of-pocket maximum.
If, however, you are seen at a network facility for non-emergency services but are unexpectedly provided services by a non-network provider, your expenses will apply to the network out-of-pocket maximum.
Let’s say that in 2017 your plan had $2,500 network and $5,000 non-network out-of-pocket maximums*. In the following example, you spent a total of $2,000 with network providers and $3,000 with non-network providers throughout the year. In 2017, any out-of-pocket expenses you paid–whether you saw a doctor in your plan’s network or not–counted toward reaching your combined out-of-pocket maximum. Your network out-of-pocket maximum counted toward your non-network out-of-pocket maximum.
Using the same example for 2018, throughout the year you spent $2,000 with network providers, which applied to your network out-of-pocket maximum; whereas, the $3,000 spent with non-network providers applied to the non-network out-of-pocket maximum. As a result, neither out-of-pocket maximum was reached for your plan by year end.
*These numbers are for example only and do not represent actual out-of-pocket maximums.
Learn more
To review these changes in detail and find your actual values for 2018, please view or download your Summary of Benefits and Evidence of Coverage.
Find out who is in your plan’s network
To check if your healthcare provider is in your plan’s network, visit blueshieldca.com/networkifpppo. We work hard to make sure our list of providers is current and accurate. However, because providers leave networks from time to time, you are encouraged to check with the provider before using their services.
Always check the network status of any provider (doctor, hospital, lab, imaging center, urgent care, etc.) before setting up an appoint. You can create a specific directory for the providers available to you in your location. https://insuremekevin.com/print-a-list-check-it-twice-for-your-health-insurance-doctors/