For Certified Insurance Agents enrolling clients into health plans through Covered California for an August 1, 2014 effective date, many have been asking why it is taking so long for the enrollment data to be transmitted to the carrier. Customer Service Representatives at Anthem Blue Cross and Covered California acknowledged on July 28th that enrollment data since the beginning of July is having a difficult time being processed by the carriers.
August enrollments delayed by IT problems
With several clients anxiously awaiting to receive their first invoice so they can activate their health plan, my calls to Covered California and the carriers were met with a standard reply of “It takes seven to ten days to process the enrollment.” A subsequent call to Anthem Blue Cross to find out if the a client’s enrollment had arrived at the carrier uncovered the truth from a frustrated CSR that they had received only a few enrollments in the month of July. In addition, IT staff at both Anthem Blue Cross and Covered California were working to resolve the issue.
Other health plans may be impacted
In retrospect, the latest enrollment data issues for Blue Shield and Health Net clients may also be the victim of the latest IT snafu plaguing Covered California. However, the representative at Covered California intimated it was the carriers who were having problems processing the Covered California data feed. As in the past, both the carriers and Covered California are pointing fingers at one another. As is also the case, agents and consumers are the last to know about the delays effecting their applications.
Consumers counting on promised August 1st start date
Regardless of who is at fault, there are numerous Californians that just want to get their health plans active. The rule is that if an individual or family applies on or before the 15th of the month their health plan will be effective the 1st of the following month when they make their initial payment. For people who have appointments scheduled shortly after the 1st of August, they could be put in jeopardy of losing those office visits or procedures. While new health plan members might be able to make their first binder payment after the 1st of the month, there can still be adelay until they receive their importantmember ID that enables them to secure health care services.
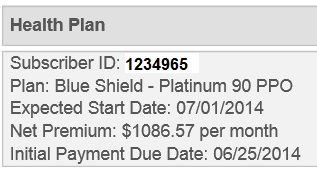
Subscriber ID is NOT a Member ID
One extra bit of information, I was informed from Anthem Blue Cross that the subscriber ID number listed on the Covered California enrollment summary of the account will now be used as another means of looking up clients. That is, of course, if the carrier actually receives the enrollment data feed. Many consumers have mistaken this subscriber ID for the actual health plan member ID. This has led to confusion on the part of consumers, agents and providers. Covered California should consider changing the name to “Tracking ID” or something that won’t be confused with an official health plan member ID.