
Complete data set of 2016 Medicare Advantage Star Ratings.
Medicare Advantage medical insurance plans and Part D Prescription Drug plans must notify existing and new members of the Centers for Medicare and Medicaid (CMS) Star Ratings that have been assigned to them. While the plans must print the overall Star Rating for the plan, there are actually over forty specific measurements, each with its own rating, that make up the overall scores. For people who want to dive deeper in to the numbers, I’ve provided the CMS spreadsheet of all the ratings for each plan and measurements.
Link to latest MA-PD Star Ratings for plan offered in 2017
2017 Medicare Advantage Star Ratings
Medicare 2016 Part C & D Star Rating Technical Notes
Along with the spreadsheet of Medicare Advantage measure ratings CMS publishes a guide of technical notes that discusses the data collection, measurements and methodology for assigning the different Star Ratings. For example, there is a Star Rating on how effective the plans are at getting members the Annual Flu Vaccine. The metric is “The percentage of sampled Medicare enrollees (denominator) who received an influenza vaccination during the measurement year (numerator).” From page 17 of the Technical Notes bulletin. This percentage number is then reported on the 2016 Report Card Master Table spreadsheet on the tab Measure Data. The Star Rating for that specific measurement is reported on the tab Measure Stars.
Download Medicare 2016 Part C & D Star Rating Technical Notes
Actual Star Measurements
We can see that contract number H0543 from United Health Care had a percentage of 75% of their members getting the Flu Vaccine for that plan in a specific county. This translates into a 4 Star Rating for the specific Flu Vaccine measurement.
2016 Medicare Advantage Star Rating Report Card
The 2016 Report Card was not designed for easy reference of location specific plans. To locate a particular Medicare Advantage plan or Part D plan you need to know the contract number. They are a five character identifier with the first character being a letter such as E for Employer, H for Local CCP, R for Regional plan, and S for Part D plans. This contract number is always listed on various marketing literature, enrollment forms and Evidence of Coverage Documents.
Download 2016 Report Card Master Table 2015
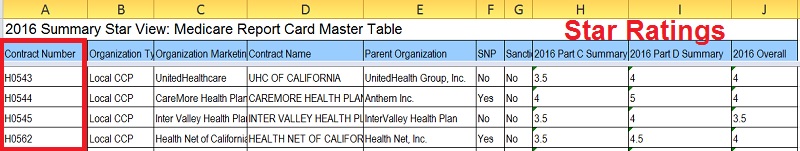
Each Medicare Advantage plan is identified by its contract number usually found on enrollment forms, marketing material, and Evidence of Coverage.
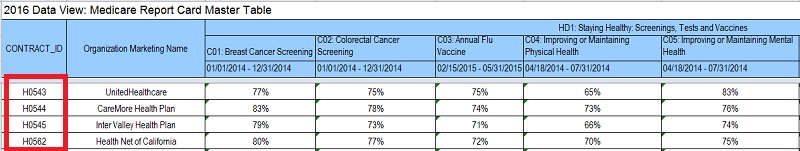
Each measurement item is given a percentage of completion which translates into a Star Rating.
The measurements are weighted differently to determine the overall Star Rating.
Summary and Overall Ratings: Weighting of Measures
For the 2016 Star Ratings, CMS assigns the highest weight to the improvement measures, followed by the outcomes and intermediate outcomes measures, then by patient experience/complaints and access measures, and finally the process measures. Process measures are weighted the least. The summary Part C, Part D, and overall MA-PD Star Ratings are calculated as weighted averages of the individual measure ratings. The weights assigned to each measure for summary and overall Star Ratings are shown in Attachment G. – page 6 of Technical Notes
Methodology for Calculating Part C and Part D Summary Ratings
The Part C and Part D summary ratings are calculated by taking a weighted average of the measure level ratings for Part C and D, respectively. To receive a Part C and/or D summary rating, a contract must meet the minimum number of individual measures with assigned Star Rating. – page 6 of Technical Notes
The overall Star Ratings are fairly comprehensive when you consider the number of different measurements CMS includes. But they also can highlight where a Medicare Advantage plan is having challenges meeting the goals of maintaining or improving the health of its members.
Data measurements included in Star Ratings
- Breast Cancer Screening
- Colorectal Cancer Screening
- Annual Flu Vaccine
- Improving or Maintaining Physical Health
- Improving or Maintaining Mental Health
- Monitoring Physical Activity
- Adult BMI Assessment
- Special Needs Plan Management
- Care for Older Adults – Medication Review
- Care for Older Adults – Functional Status Assessment
- Care for Older Adults – Pain Assessment
- Osteoporosis Management
- Diabetes Care – Eye Exam
- Diabetes Care – Kidney Disease
- Diabetes Care – Blood Sugar
- Controlling Blood Pressure
- Rheumatoid Arthritis Management
- Reducing the Risk of Falling
- Plan All – Cause Readmissions
- Getting Needed Care
- Getting Appointments and Care Quickly
- Customer Service
- Rating of Health Care Quality
- Rating of Health Plan
- Care Coordination
- Complaints about the Health Plan
- Members Choosing to Leave the Plan
- Beneficiary Access and Performance Problems
- Health Plan Quality Improvement
- Plan Makes Timely Decision about Appeals
- Reviewing Appeals Decisions
- Call Center – Foreign Language Interpreter and TTY
- Appeals Auto-Forward
- Appeals Upheld
- Complaints about the Drug Plan
- Drug Plan Quality Improvement
- Rating of Drug Plan
- Getting Needed Prescriptions
- MPF Price Accuracy
- High Risk Medication
- Medication Adherence for Hypertension
- Medication Adherence for Cholesterol
- Medication Therapy Management Completion Rate for CMR
2016 High Performers 5 Stars
| Contract Number | Organization Type | Organization Marketing Name | Rated As | Highest Rating | Rating |
| H0354 | Local CCP | Cigna | MA-PD | Overall | 5 |
| H0524 | Local CCP | Kaiser Permanente | MA-PD | Overall | 5 |
| H0630 | Local CCP | Kaiser Permanente | MA-PD | Overall | 5 |
| H1230 | Local CCP | Kaiser Permanente | MA-PD | Overall | 5 |
| H1651 | 1876 Cost | Medical Associates Health Plan, Inc. | MA-Only | Part C Summary | 5 |
| H2150 | 1876 Cost | Kaiser Permanente | MA-PD | Overall | 5 |
| H2256 | Local CCP | Tufts Health Plan or Tufts Medicare Preferred | MA-PD | Overall | 5 |
| H2462 | 1876 Cost | HealthPartners | MA-PD | Overall | 5 |
| H2610 | Local CCP | Essence Healthcare | MA-PD | Overall | 5 |
| H5256 | 1876 Cost | Medical Associates Clinic Health Plan of Wisconsin | MA-Only | Part C Summary | 5 |
| H5262 | Local CCP | Gundersen Health Plan, Inc. | MA-PD | Overall | 5 |
| H5264 | 1876 Cost | Dean Health Plan, Inc. | MA-Only | Part C Summary | 5 |
| H5591 | Local CCP | Martin’s Point Generations Advantage | MA-PD | Overall | 5 |
| H5652 | Local CCP | Erickson Advantage | MA-PD | Overall | 5 |
| H9003 | Local CCP | Kaiser Permanente | MA-PD | Overall | 5 |
| S0655 | PDP | Tufts Health Plan Medicare Preferred | PDP | Part D Summary | 5 |
| S5753 | PDP | WPS Health Insurance | PDP | Part D Summary | 5 |
2016 Low Performers
| Contract Number | Organization Type | Organization Marketing Name | Rated As | 2016 C Summary | 2016 D Summary | Reason for LPI |
| H1903 | Local CCP | WellCare | MA-PD | 3 | 2.5 | Part C or D |
| H2905 | Local CCP | Sierra Health and Life Insurance Company, Inc. | MA-PD | 2.5 | 3.5 | Part C |
| H3327 | Local CCP | Touchstone Health | MA-PD | 3 | 2.5 | Part C or D |
| H4866 | Local CCP | Access Medicare | MA-PD | 2 | 3 | Part C |
| H5698 | Local CCP | WellCare | MA-PD | 2.5 | 3 | Part C |
| H6801 | Local CCP | Blue Cross Blue Shield of Oklahoma | MA-PD | 2.5 | 3.5 | Part C or D |
Fact Sheet – 2016 Star Ratings
One of the Centers for Medicare & Medicaid Services’ (CMS) most important strategic goals is to improve the quality of care and general health status for Medicare beneficiaries. CMS publishes the Part C and D Star Ratings each year to: measure quality in Medicare Advantage (MA) and Prescription Drug Plans (PDPs or Part D plans), assist beneficiaries in finding the best plan for them, and determine MA Quality Bonus Payments. Moreover, the ratings support the efforts of CMS to improve the level of accountability for the care provided by physicians, hospitals, and other providers. CMS continues to see increases in the number of Medicare beneficiaries in high-performing Medicare Advantage (MA) plans. Star Ratings are driving improvements in Medicare quality. The information included in this Fact Sheet is evidence of such improvement and is based on the 2016 Star Ratings published on Medicare Plan Finder (MPF) on October 8, 2015.
Background
Medicare Advantage with prescription drug coverage (MA-PD) contracts are rated on up to 44 unique quality and performance measures; MA-only contracts (without prescription drug coverage) are rated on up to 32 measures; and stand-alone PDP contracts are rated on up to 15 measures. Each year, CMS conducts a comprehensive review of the measures that make up the Star Ratings, considering the reliability of the measures, clinical recommendations, feedback received from stakeholders, and data issues. All measures transitioned from the Star Ratings are included in the display measure available from this page http://go.cms.gov/partcanddstarratings. Changes to existing measures are summarized in Attachment A.
The Star Ratings measures span five broad categories:
- Outcomes
- Intermediate Outcomes
- Patient Experience
- Access
- Process
For the 2016 Star Ratings, outcomes and intermediate outcomes continue to be weighted three times as much as process measures, and patient experience and access measures are weighted 1.5 times as much as process measures. CMS assigns a weight of 1 to all new measures. The Part C and D quality improvement measures receive a weight of 5 to further reward contracts for the strides they made to improve the care provided to Medicare enrollees. CMS continues to lower the overall Star Rating for contracts with serious compliance issues, defined as the imposition of enrollment or marketing sanctions.
Highlights of Contract Performance in 2016 Star Ratings
Changes in Ratings from 2015
The last row in Table 1 details the trend in the average overall Star Ratings weighted by enrollment for MA-PDs for the period of 2013 to 2016.
- Approximately 49 percent of MA-PDs (179 contracts) that will be active in 2016 earned four stars or higher for their 2016 overall rating.
- This is nearly a 9 percentage point increase from 40 percent of active contracts earning four stars or higher for their 2015 overall rating.
- Weighted by enrollment, close to 71 percent of MA-PD enrollees are in contracts with four or more stars.
- This is nearly an 11 percentage point increase from 60 percent of enrollees in contracts with four or more stars in 2015.
- Approximately 41 percent of PDPs (24 contracts) that will be active in 2016 received four or more stars for their 2016 Part D rating.
- Weighted by enrollment, close to 32 percent of PDP enrollees are in contracts with four or more stars.
Download 2016 Star Rating Fact Sheet